We share an opinion article by nurse Marta Pires, in which she explains the role of the nurse in the palliative approach to people with dementia.
Although based on the same principles as Palliative Care in general, Palliative Care for the Elderly must take on some specificities, taking into account the complexity of the elderly and the impact that clinical problems can have on their frailties. The European Union Geriatric Medicine Society defined the concept of Geriatric Palliative Care as “the provision and management of medical care for elderly people suffering from problems associated with progressive and advanced disease, with a limited prognosis, with the aim of improving quality of life” (Pereira, 2014, p.295, citing Pautex et al., 2010).
In practice, there is still a great undervaluation of the elderly as recipients of Palliative Care, possibly because death is more expected. This devaluation is reflected in aspects such as: less access to emotional and spiritual support in the last days of life, less support in the assessment and control of pain, poor participation in therapeutic decisions and in the choice of place of death (their opinions are not taken into account) (Lloyd et al., 2016). In the case of people with dementia, the devaluation is even more evident, possibly due to the difficulty in assessing the person’s suffering; in addition, symptomatic control may be hampered “by the fact that they express themselves poorly verbally and also by the mistaken idea that this type of patient does not experience pain or other symptoms, although the available evidence shows that this idea is incorrect” (Neto, 2016, p.491). These aspects are reflected in the difficulty of health professionals in recognizing their palliative needs and adapting a care plan to each situation (Lloyd-Williams, Mogan and Dening, 2017). This complexity requires a multidisciplinary and multidimensional approach, starting with the assessment of the (specific) capabilities and needs of each person.
Care for people with dementia includes integrated and systemic interventions, both pharmacological and non-pharmacological, with emphasis on the family and psychosocial approach (Fernandes, 2014). According to Guedes (2014), around 43% of elderly people live with their families, which contradicts the lack of investment in the family as a care provider, and simultaneously supports the need to support elderly people and their families in the community. This is a challenging aspect for Nursing, considering that the nurse is a close-knit professional with the ability to assess and intervene in the person, in all dimensions and in all care contexts.
According to the Palliative Nursing Group of the Royal College of Nursing, referred to by Magalhães (2009), the role of palliative nursing involves assessing the needs of the sick person and their family – in terms of physical, psychological, social and spiritual health – and planning, implementing and evaluating appropriate interventions with the aim of promoting quality of life and a dignified death. Thus, in all care contexts, nurses must be able to provide support and comfort to the sick person, value them, maintain hope, preserve dignity, be present, be empathetic, know the patient and family (target of care) well and have the ability to keep up to date with their knowledge, thus ensuring the quality and sustainability of their interventions (Jacono, 2009).
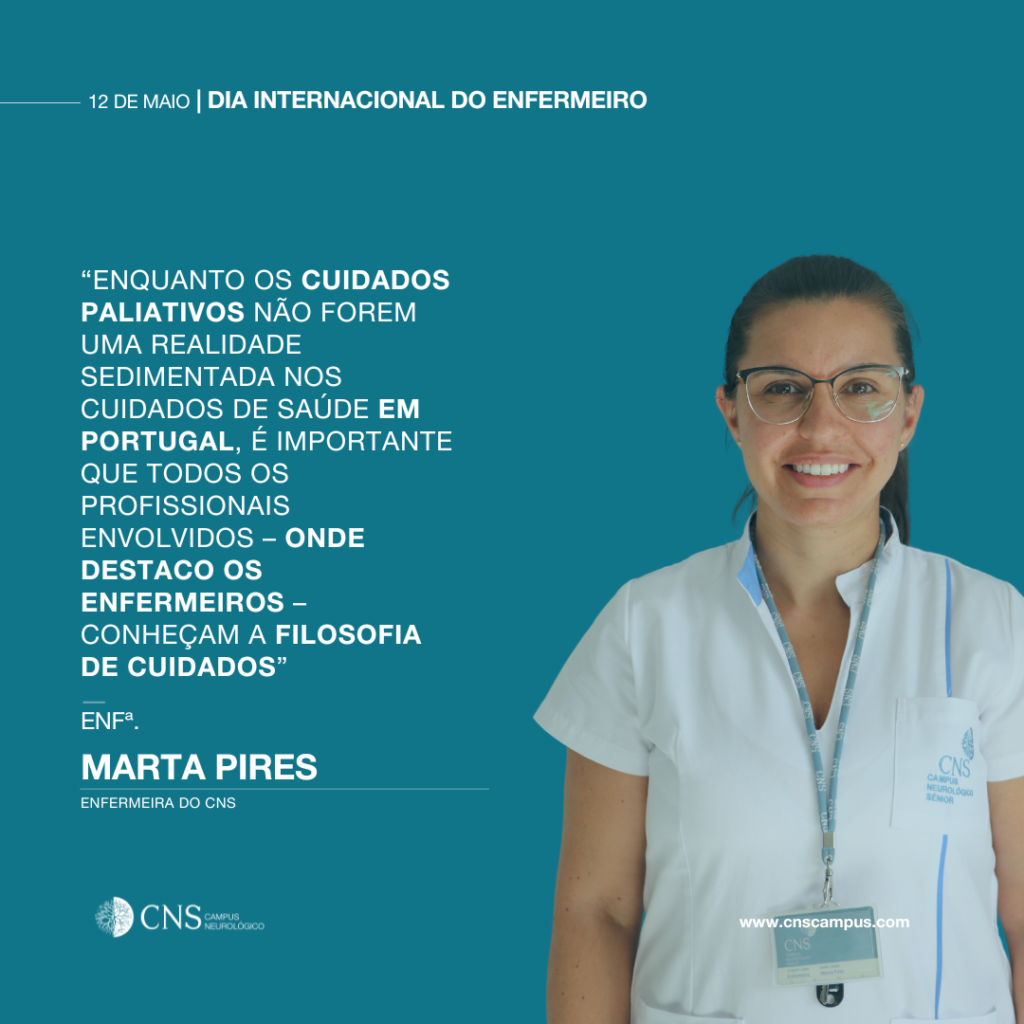
While palliative care is not a well-established reality in healthcare in Portugal, it is important that all professionals involved – and I would like to highlight nurses – are familiar with the philosophy of care to ensure adequate continuity of care throughout the course of the disease and develop skills to intervene, at least, with palliative actions, considering the pillars of the palliative approach. The road ahead is long and challenging for nurses, but awakening them to these issues – which would probably be the most difficult step – is already happening and, more importantly, is in line with the holistic and interpersonal nursing that has been taught from the beginning. Let’s keep going!
Marta Pires, Nurse at the CNS – Neurological Campus